

Normally, a person has 46 chromosomes, each of which are made up of thousands of genes, which are located inside all cells in the body. What is Down syndrome?ĭown syndrome, also called trisomy 21, is the most common chromosomal abnormality in newborns, occurring in about one of every 700 births. Note that screening tests cannot diagnose or rule out specific conditions so a screen negative result does not mean your baby will not be born with Down syndrome, it means that the chances are low. Your integrated screening results are considered "screen negative" if the risk for Down syndrome is less than one in 110 (for example, 1 in 150 or 1 in 200). What does a negative result for Down syndrome mean? It's important to note that five out of every 100 women who take the integrated screening test receive "screen positive" results but most will not have a baby with Down syndrome. We will then offer you an amniocentesis test to examine your baby's chromosomes. If your results are "screen positive," your baby has a higher risk for Down syndrome than other babies. Your integrated screening results are considered "screen positive" if the risk for Down syndrome is one in 110 or greater (for example, 1 in 90 or 1 in 80). What does a positive result for Down syndrome mean?

We send a copy of the test results to your physician and a genetic counselor will call you to discuss the results and schedule any necessary follow-up appointments. We can also use the screening results to estimate the risk for other disorders including open neural tube defects (spina bifida) and Trisomy 18.The integrated screening results are usually ready one week after the second stage. The NT measurement, the levels of the five substances in your blood and your age help us estimate your risk of having a baby with Down syndrome. We combine the results from the first and second stages into a single screening result.

The test is performed at the Prenatal Diagnosis Center in two stages: There are different ways to test for Down syndrome screening but the Integrated Test is the most specific, has the highest detection rate and a low false-positive rate. Centrifuge and aliquot serum into a plastic vial within 2 hours of collection.The Integrated Screening Test tells you what the chances are that your baby might have Down syndrome or open neural tube defects such as spinal bifida. The ultrasound and blood draw must be completed within a gestational window of 10 weeks, 0 days and 13 weeks, 6 days, which corresponds to a crown-rump length range of 31 to 80 mm.Ģ. Complete the NT/CRL Data for First Trimester/Sequential Maternal Screening.ġ. See Maternal Screening: Sonographer Approval Process. Do not send specimen to Mayo Clinic Laboratories if the sonographer is not NT-certified or before completing the application process.
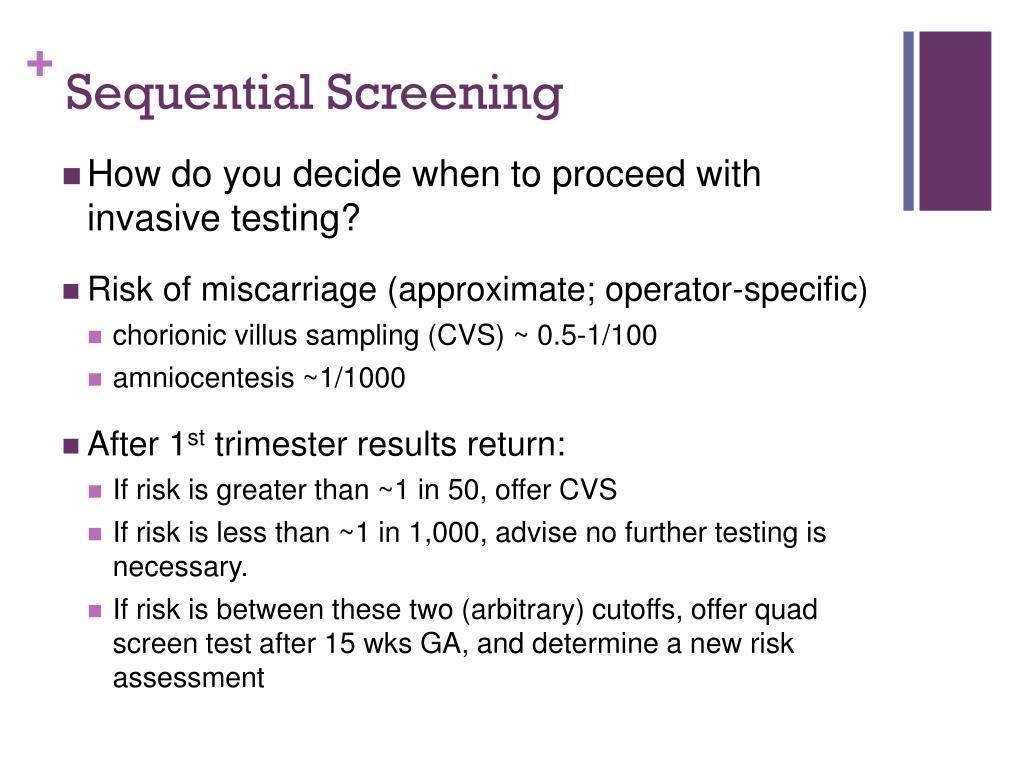
Nuchal translucency (NT) measurements are only accepted from NT-certified sonographers. Sequential maternal screening is a 2-part test that includes a first-trimester sample (this test) and a second-trimester sample (SEQB / Sequential Maternal Screening, Part 2, Serum).Īpproval to send specimen for first-trimester screening is required and may take up to 5 business days to complete. If a stand-alone neural tube defect risk assessment is desired, order MAFP1 / Alpha-Fetoprotein (AFP), Single Marker Screen, Maternal, Serum. If collecting a second-trimester specimen is expected to be difficult, order first-trimester screening instead (1STT1 / First Trimester Maternal Screen, Serum). When part 1 is negative, part 2 must be completed in order to receive an interpretable result.


 0 kommentar(er)
0 kommentar(er)
